Peripheral Neuropathy and Statins
Question: Can something be done to slow the progression.
Physicians’ offices now post a sign in their patient rooms. It reads:
Questions to ask your doctor:
What is my problem?
What do I need to do about it?
Why do I need to do this?
I applied these questions to my husband’s peripheral neuropathy because it is getting worse.
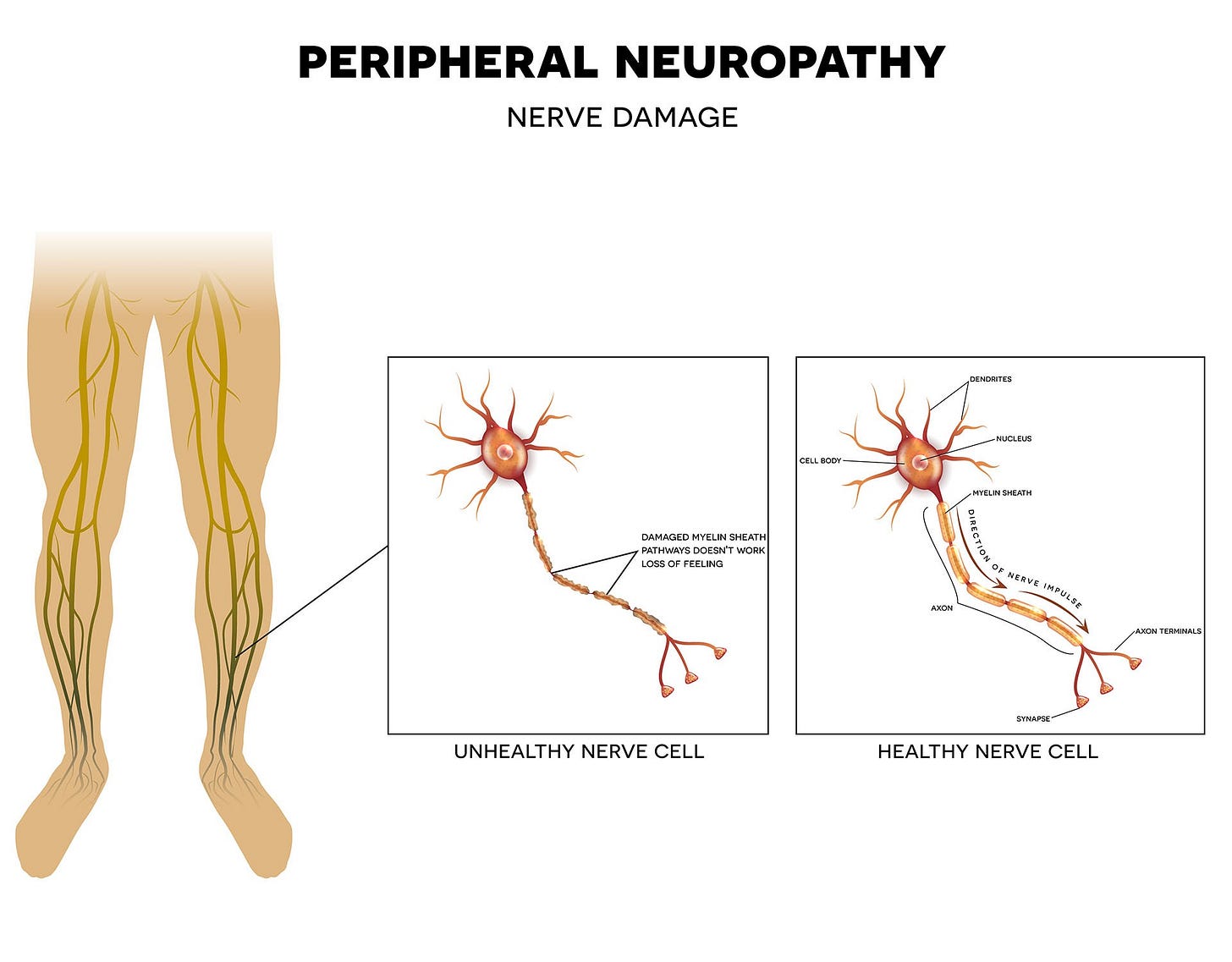
The health problem is peripheral neuropathy. The continued questioning and examination of this problem is important because there may be ways to mitigate his discomfort. We need to do this because the progression discussed below is quite scary.
My husband’s peripheral neuropathy was diagnosed five years ago. He describes his symptoms as numbness in his feet and ankles, noting, “it is not really pain, more of an ache.” It worsens throughout the day. The ache, which for some peripheral neuropathy sufferers is pain, extends from his feet up to his calf. The feeling is relieved with rest, Tiger Balm, or SalonPas, and a massage of the feet and ankles. It never disappears.
We both had accepted his neurologist’s statement two years ago, “We don't know what's causing this: call me if it gets worse.” But, last week, I read that peripheral neuropathy can lead to life in a wheelchair and amputation. I think we need to do something more proactive because the consequences are so severe.
Peripheral neuropathy has four stages. Interesting, our doctor never mentioned this as a staged problem with possible consequences! Perhaps he did not want to worry us. The neurologist did indicate that some people do not see advancement of the disease. He also stated that the cause of peripheral neuropathy is not yet known.
I found information about the four stages on physician sites and through a Google AI search. Aurora Health Care defined Stage 2:
“It's more noticeable and consistent, and it cannot be ignored because it is now impacting a few other things and requires the patient to interrupt daily tasks.”
This description matches my husband’s symptoms and behavior. For example, he cannot stand for two to three hours without needing to rest. Google AI pointed me to the New York Presbyterian Hospital website, which described Stage 4:
“You feel complete numbness and loss of sensation in your hands and feet; the risk of amputation increases.”
I sifted through internet material about peripheral neuropathy. There are articles from scientific research papers made available online, as well as, some from reputable sites, such as the Mayo Clinic. There are many YouTube videos about peripheral neuropathy by physicians, including Dr. Mark Hyman, founder of the Cleveland Clinic Center for Functional Medicine.
There are numerous connections between peripheral neuropathy and medications, as well as other factors. On the Foundation for Peripheral Neuropathy website, there is a recorded webinar about hereditary neuropathy and genetic testing.
My husband’s twenty-five-year history with statins and the fact that his dose of atorvastatin increased by ten milligrams six years ago, influenced my decision to do further research. I am looking for studies that support the connection between statins and peripheral neuropathy. There are many case studies, like one on the Foundation for Peripheral Neuropathy website. It discusses a man who removed statins and alleviated symptoms of neuropathy.
The reason statins may cause peripheral neuropathy was indicated on the People’s Pharmacy Website, The People's Perspective on Medicine states
“It turns out that nerve cells need cholesterol. A recent study from Heidelberg, Germany, demonstrated a link between low LDL cholesterol and neuropathy in people with type 2 diabetes (JAMA Network Open, May 31, 2019). The authors suggest that nerves can’t repair themselves when cholesterol is too low.”
Are there conclusive studies that statins cause neuropathy? After reading the above article and reviewing others, the answer is No. However, there is sufficient evidence that we should investigate my husband’s specific situation. The National Library of Medicine reprints an article that points to atorvastatin. The article is titled, “Peripheral polyneuropathy in patients receiving long-term statin therapy.” Here is the abstract:
“Peripheral neuropathy is an important potential side effect of statin use. This study was an investigation of the incidence of peripheral neuropathy in patients taking atorvastatin or rosuvastatin for hypercholesterolemia and the relationship to the dose and duration of the treatment.”
To potentially prevent any further damage, I am going to make an appointment with my husband’s doctor to see if he can try alternative cholesterol-lowering medications: non-statins. But first, I think we should request a complete liver panel to determine if there are any indications of liver problems. (Note, you can get a liver panel without a doctor’s order by paying the fee directly to Lab Corps and booking an appointment.)
With all the google doctoring I do, I regret not searching this one out and asking more questions. I think society has blind faith in physicians and medicines that need heavier scrutiny. Physicians are overwhelmed in this current post-COVID world (which really isn’t post-COVID because it is still classified as a pandemic) and there are numerous approaches to health conditions that are resisted when they do not fit the traditional paradigms.
Other Resources: